- | 9:00 am
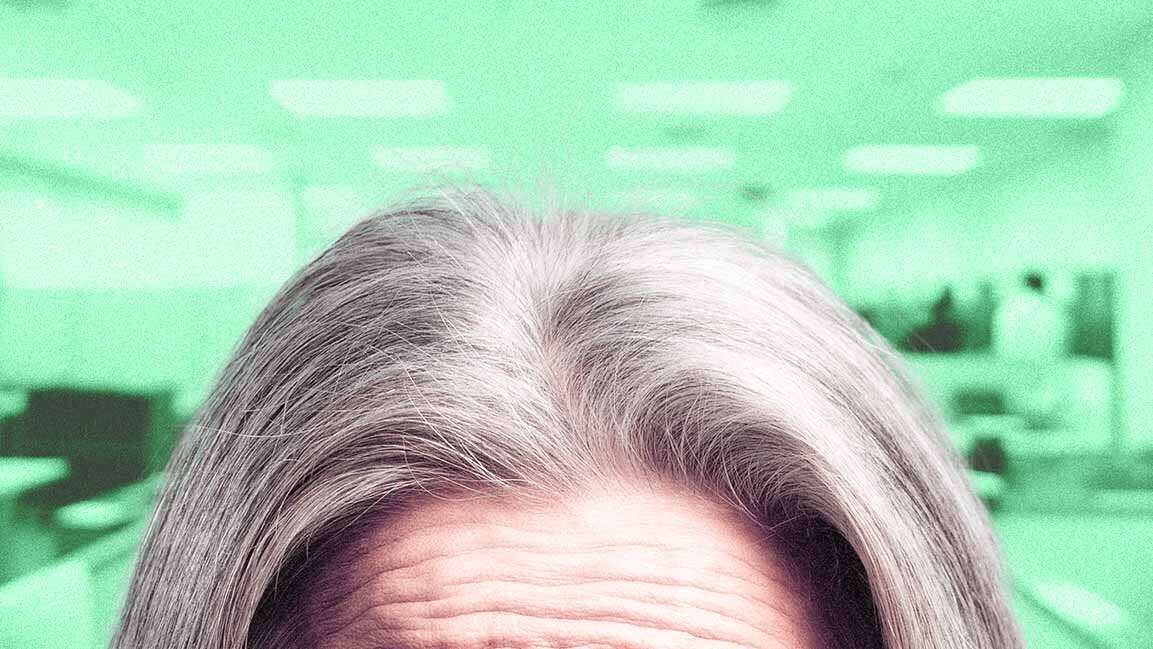
How the pressure to be ‘picture-perfect’ is silencing MENA youth on mental health
Cultural factors such as social reputation, family dynamics, and stigma are preventing many from being open about their mental health struggles.

For the past few years, mental health campaigns have focused on normalizing mental illness—encouraging people to talk about their feelings and get help if they need it.
In the Middle East and North Africa (MENA), where social and cultural barriers have long made mental health difficult to discuss, there’s a newfound openness online. For many young people, the digital space feels safer. In person, however, silence often returns, weighed down by stigma and the lack of anonymity.
A recent report spanning 16 countries across Asia and the Middle East reveals how much the medium of conversation matters. When surveys are conducted online, young people appear less happy than older generations. But switch to phone calls or face-to-face interactions, and the story flips: the young emerge as the most optimistic and least burdened by negative emotions.
A CULTURE BASED ON COMMUNITY
Khaled Salaheldin, psychotherapist at Up Therapy and Well-being, explains that the MENA region’s culture often prioritizes social reputation over individual emotional needs—shaping how young people express distress and seek help.
“Patriarchal family structures often place fathers and extended relatives in charge of health decisions, limiting adolescents’ autonomy and encouraging suppression or physical expression of psychological symptoms to avoid shame,” he says.
Mira Shaker, a psychotherapist, notes that Egypt, like many countries in the region, values strength. This makes it difficult for individuals to seek help for emotional struggles without feeling as though they are admitting weakness. Many Egyptian youth, particularly men, end up suffering in silence, coping through avoidance, overworking, or distraction.
“In my clinical experience, social desirability bias often appears as a need to seem strong and morally upright. Because emotional control and family loyalty are highly valued,” Shaker says, adding that many tend to hide their distress, avoid discussing family issues, or downplay emotions they perceive as shameful.
“Ultimately, these cultural patterns shape collective attitudes toward mental health. Therapy often begins with relearning that emotions are not threats to strength, but essential experiences of humanity and connection.”
Ehab Youssef, a Psychology AI researcher and a computational-clinical psychotherapist, adds that in many MENA societies, identity is deeply relational. “A young person isn’t simply someone who happens to have a family, but someone whose very selfhood is woven through family connections,” he says.
When emotional distress arises, it often becomes intertwined with family welfare. Research across Egypt, Lebanon, Jordan, and Gulf states reflects this pattern. Youssef notes that gender plays a major role: “Young women face stricter monitoring around modesty and reputation, while young men face pressure to be strong and never show vulnerability because ‘men don’t cry.’”
Studies consistently document higher rates of physical symptoms expressing psychological distress in Middle Eastern populations—genuine pain carrying emotional weight.
SOCIAL MEDIA AMPLIFICATION
Social media often intensifies the pressure to present an idealized self, which can take a toll on mental well-being. Shaker explains that while these platforms enable connection and self-expression, they reinforce cultural expectations to appear strong, successful, and emotionally composed.
“Many youth feel compelled to display an idealized version of themselves, emphasizing social status, appearance, and achievements,” she says. “In a society that highly values reputation and family image, this digital performance can worsen existing norms around social comparison and emotional restraint.”
Constant exposure to curated lives can create unrealistic standards, leaving many feeling inadequate or behind. Shaker adds, “Over time, internalizing the belief that vulnerability should be hidden weakens emotional openness and self-compassion, making seeking professional help feel less acceptable and more like a threat to exposure.”
Social media has intensified existing cultural pressures, adding new digital dimensions to long-standing norms around reputation and self-presentation, says Youssef. Research shows correlations between heavy social media use and increased anxiety, depression, and body image concerns, though causation remains complex.
In MENA cultures rooted in honor-based values, reputation management has always been central—but now the scale and permanence have multiplied. Youssef says, “The same young person navigating family expectations offline must now manage an Instagram balancing self-expression with family values, a Snapchat fitting peer expectations, a Twitter navigating political sensitivities, a TikTok that’s current but not ‘too much,’ a LinkedIn for professional presentation.”
The constant comparison across these platforms exposes youth to conflicting ideals—from traditional family expectations to global celebrity standards. Yet, Youssef says, not all effects are negative.
Many young people use social media to find supportive communities, access mental health information, engage in activism, and express creativity. “Research suggests how platforms are used matters more than how much—active engagement may be less harmful than passive scrolling,” he says.
“This digital amplification of existing pressures intersects with the existing cultural dynamics and research challenges. Those already hesitant to report distress now compare themselves to others appearing perfectly fine on social media, minimizing their struggles. The interventions needed must address this layered reality.”
DIAGNOSIS AND TREATMENT
Salaheldin says that in conservative cultures, young people often underreport experiences of depression, anxiety, substance use, or family conflict.
“Clinically, this bias can delay accurate diagnosis, disrupt the therapeutic alliance, and drive early dropout when the gap between the presented self and lived experience becomes untenable,” he says. It can be intentional (impression management) or unintentional (self-deception), with some youth consciously hiding stigmatized thoughts or behaviors while others struggle to recognize experiences that conflict with culturally prescribed narratives about mental health, he adds.
Widespread stigma continues to undermine both research quality and clinical care. Studies that attribute treatment gaps of up to 90% to shame and fear of social rejection.
“In studies, stigma-driven social desirability bias leads to underreporting of symptoms, risks, and needs, skewing prevalence estimates and intervention design,” says Salaheldin. “Surveys in Arab countries show pronounced bias around sensitive topics. Clinically, families often turn first to traditional or religious healers, delaying evidence-based care, while shame and disclosure fears limit engagement once treatment begins.”
Youssef notes that stigma toward mental illness remains higher in MENA populations compared to Western samples, with social desirability significantly affecting self-reported data. However, he says, the extent of underreporting remains unclear.“A young person experiencing what would clinically qualify as significant depression might rate their distress as mild. Why? Because compared to those who are ‘really sick,’ their problems seem minor,” Youssef explains.
“Meanwhile, a Western youth with similar symptoms might rate their distress higher—not because they’re suffering more, but because their cultural context permits acknowledging it.”
He warns that underestimating the prevalence of mental health issues has wide-reaching consequences: resources are misallocated, young people feel isolated, and prevention programs remain underdeveloped, perpetuating the silence.
Treatment outcomes also suffer, he adds, as most evidence-based therapies assume Western norms of individuality, verbal expression, and strict confidentiality. “Effective treatment in the MENA region may instead require family involvement, multiple forms of expression, and strategic transparency,” he says. Some clinicians, he adds, are already adapting proven therapies to local contexts by integrating indigenous healing practices.
Current research is constrained by measurement gaps and cultural bias, underscoring the need for local studies that reflect young people’s lived experiences. “Yet clinical experience offers hope. When young people access culturally responsive, genuinely empathic care, they respond,” adds Youssef.
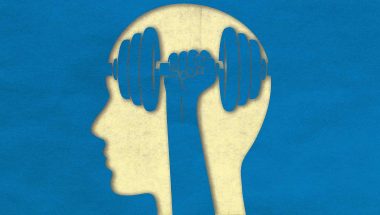
NEEDED INTERVENTIONS
Salaheldin notes that when therapy is tailored to local culture, it works better. “That can mean using everyday language and familiar expressions, acknowledging religion and using faith-friendly examples, involving families with clear education and practical skills, and using stories and visuals that feel relevant,” he says.
Cognitive behavioral therapy, acceptance and commitment therapy, motivational interviewing, dialectical behavior therapy skills, narrative therapy, and private online CBT are beneficial for Arabic-speaking youth and refugees.
Reducing stigma, Salaheldin adds, is key to accessibility. “Helpful steps include clear, friendly education that explains mental health as a mix of biology and environment, hearing from peers with similar experiences, school programs that make support easy to find, culturally authentic videos on social media, and partnerships with religious and community leaders.”
Effective interventions must address the interconnected challenges, cultural dynamics that complicate authentic expression, research and treatment approaches that often don’t fit MENA contexts, and digital pressures amplifying existing struggles, says Youssef.
“The goal isn’t extracting young people from their contexts but supporting them in living with integrity within them.”
Youssef says the region must build accessible mental health systems by ensuring therapeutic spaces where youth feel safe sharing emotional truths, developing an emotional vocabulary for young people who often lack language for their inner experiences, and involving families as allies, since most youth seek connection rather than separation.
“Education for families must resonate with their values. Rather than ‘your child has a mental illness,’ try ‘your child is experiencing stress affecting their health and happiness.’”
Youssef further highlights the need for school—and community-based interventions, digital wellness education, and the integration of multiple healing traditions.
“Effective approaches might thoughtfully combine modern therapeutic techniques with religious or spiritual counseling, traditional practices, family involvement, and community support—not choosing between Western or traditional, but integrating what works.”
Finally, Youssef notes that an essential element is simply witnessing someone’s struggle, which is real and worthy of care.
“When a young person experiences even one relationship where they don’t have to perform, where their full truth is welcome, where acceptance doesn’t depend on being who others need them to be, something fundamental shifts. That’s not liberation from culture; its liberation within and through relationships, addressing all the challenges these young people face in a complex, interconnected world.”