- | 9:00 am
Tech is rewiring Middle Eastern healthcare into a truly patient-centric model
Personalized digital tools are creating a unified and democratized healthcare infrastructure
As Middle Eastern countries strive to strengthen their healthcare systems, the adoption of advanced technologies has become crucial for maintaining a competitive edge.
Deloitte reports that AI and robotics are rapidly reshaping the sector. In the UAE and Saudi Arabia, major national initiatives are accelerating investment in digital health infrastructure and services. The UAE’s Centennial 2071 Plan and Artificial Intelligence Strategy 2031 have positioned the country as a hub for medical innovation and health tourism. Saudi Arabia’s Health Sector Transformation Program aims to provide inclusive services to 88% of the population and implement unified digital medical records nationwide by 2025.
Qatar, Kuwait, Oman, and Bahrain, are also expanding the use of AI and robotics to enhance healthcare delivery. Collectively, these efforts are driving substantial progress in patient-centric care across the region.
THE IMPACT OF TECH
Mohamed El Missaoui, CEO of Bupa CareConnect, says that adopting a modern healthcare model that integrates technology and clinical expertise within a single ecosystem enables a more transparent, proactive, and personalized patient experience. He highlights his organization’s recent tripartite agreement with NEOM and Oura to develop a digital health system based on data and predictive analytics.
“This partnership enables beneficiaries to track their health and improve their lifestyle habits while allowing healthcare providers to monitor potential risks and intervene early to reduce them,” he says.
Digital tools are helping redesign healthcare around the patient rather than the institution. Mina Shawky, Co-founder and CEO of CliniDo, says, “AI increases the speed and precision of disease detection, personalized decision-making, and automates time-consuming administrative steps—reducing waiting times and improving access.”
Telemedicine has become particularly transformative in areas where geographic or socioeconomic barriers limit specialist care. “These digital touchpoints give patients more control, greater convenience, and continuous support—ultimately creating a more inclusive and patient-centric care model,” adds Shawky.
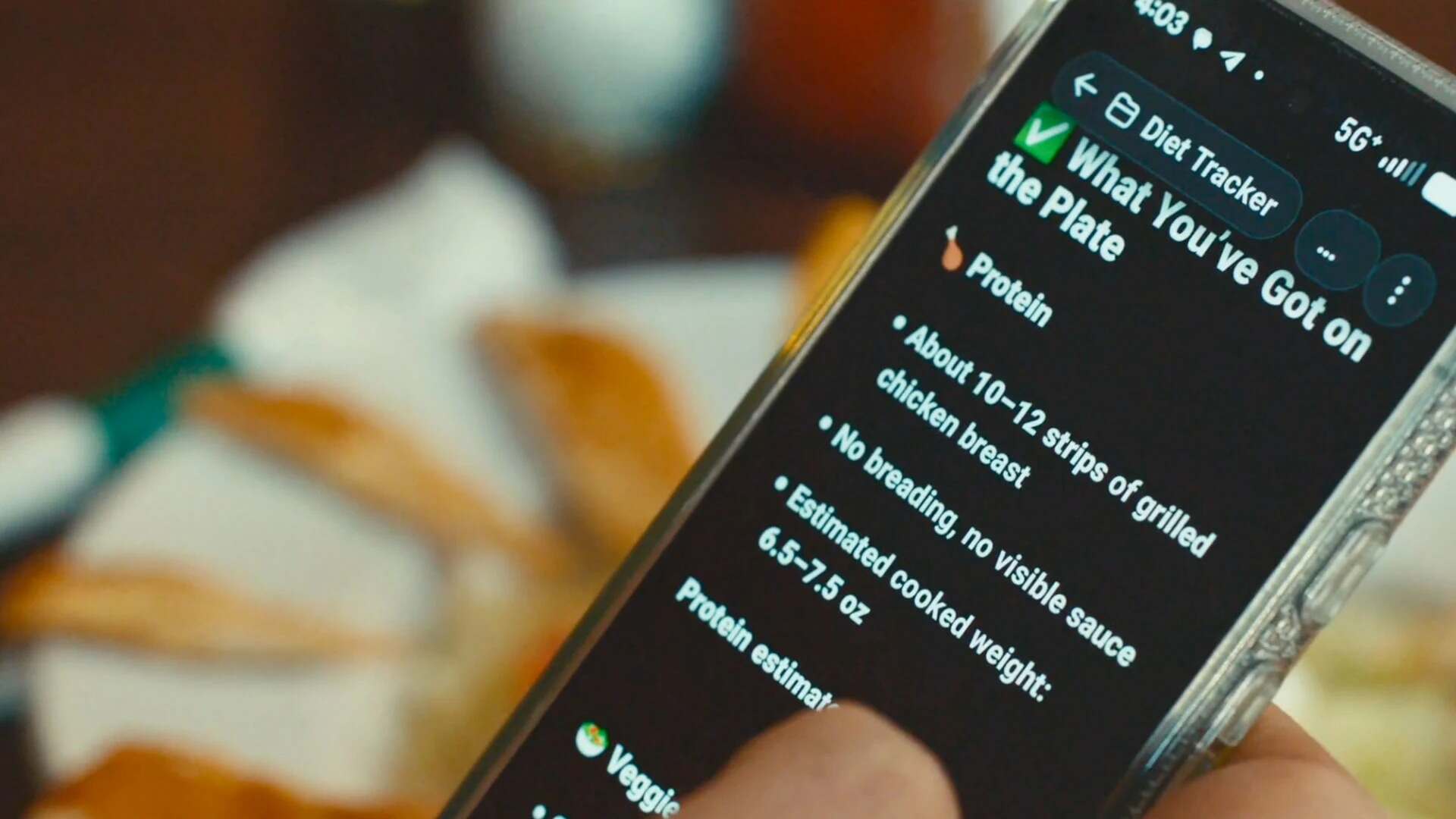
Technology enhances patient empowerment, with wearables and remote monitoring enabling individuals to take greater control of their health data and facilitate more effective daily health management. Dr. Khatija Ali, founder of BioSapien, notes that patient-centric systems benefit from integration, where tools such as wearables, telemedicine, in-clinic visits, and diagnostics all contribute to a unified care journey.
“This allows better coordination across care settings (hospital, outpatient, home), reducing duplication, improving hand-offs, and focusing on the patient’s experience rather than system convenience.”
Ali also notes that bringing care closer to patients reduces the overall burden by enabling self-management, remote follow-up, and improved adherence and outcomes.
Meanwhile, technology has advanced to the point where healthcare can become genuinely personal. Dr. Harpreet Sood, Co-Founder and Medical Director of Skai Health, says, “The breakthrough is not in apps or gadgets. It is in the intelligence that restores the human connection.”
He points to tools such as AI scribes that “listen, understand, and give time back to the clinician and patient,” as well as wearables like smart rings, sleep trackers, and continuous monitors that generate real-time data to guide tailored advice and treatment.
“These medically approved tools are flagging early signals before symptoms appear and helping us deliver care that does not wait for illness. Today, people often move across borders, and these tools create continuity with your health story, travelling with you.”
THE POWER OF PARTNERSHIPS
Strong collaborations across insurers, hospitals, and tech players are crucial to enabling health ecosystems to make a smooth transition towards value-based, coordinated, and accessible care. “Hospitals bring clinical expertise and a direct touch to the patient, while technology companies create the digital platforms on which scheduling, communications, data flows, and monitoring are made seamless,” Shawky says.
“When the insurers join the ecosystem, they are better positioned to incentivize care prevention and make essential services more affordable.”
Shawky says CliniDo’s partnerships have already improved patient access by streamlining appointment bookings and providing clearer visibility into provider availability.
Ali says collaborations are essential to bringing patient-centric solutions to market at scale. In BioSapien’s case, hospitals play a key role by integrating the implant into existing oncology pathways, validating its clinical benefits, and training clinicians to use it as a targeted alternative to systemic chemotherapy.
“This shifts cancer care toward a model that reduces toxicity, shortens recovery time, and improves day-to-day quality of life — all core pillars of patient-centric treatment.”
She adds that insurers and technology partners also help ensure the innovation is accessible and sustainable, while tech companies provide the data, monitoring capabilities, and digital tools needed to personalize care and track outcomes in real-time.
El Missaoui outlines how partnerships have supported Bupa CareConnect’s digital transformation. Collaborations with the Public Investment Fund (PIF), SABIC, the National Housing Company (NHC), and other entities have enabled the organization to establish on-site clinics offering general medicine, physiotherapy, occupational health, and emergency services, as well as wellness and mental health programs to enhance employee well-being. The approach brings healthcare directly to workplaces, increasing accessibility for employees.
“These partnerships also enable Bupa CareConnect to expand its digital ecosystem through a unified infrastructure that integrates all aspects of care within one connected system, enhancing operational efficiency and elevating service quality,” he says.
According to Sood, true collaboration involves insurers investing in continuous primary care, as accessible prevention reduces claims, and hospitals working with them, because upstream management of chronic conditions eases pressure on emergency departments. Tech companies, he adds, are also realizing that healthcare requires clinical credibility, regulatory awareness, and patience. When these efforts align around proactive diagnostics and prevention, the entire model begins to shift.
In the coming years, he adds that healthcare will be built through partnerships that reward wellbeing, not illness. “What we do not want to do is copy Western models but build something uniquely regional — combining world-class clinical science with the hospitality and discretion that define the Gulf.”
SECURITY AND PRIVACY
Data security and privacy remain major concerns in any large-scale technology integration, particularly in a sector as sensitive as healthcare.
“More healthcare providers need to ensure that data security and patient privacy are taken seriously. It also requires providers to invest in capabilities and infrastructure, and not just see this as a one-off cost,” says Sood.
He notes that much of this comes down to clarity, transparency, and accountability, and ensuring that all partner providers work with commitment to these basic principles.
“Patients also need to know exactly how their data is being used, for what purposes, and being shared with whom to guide their care.”
Ensuring data security and patient privacy requires embedding protection at every layer of the digital workflow.“This includes using encrypted cloud infrastructure, role-based access controls, secure identity verification, and regular cybersecurity audits,” says Shawky. “Adhering to international regulations on information security, such as GDPR or its regional equivalents, is another important component in keeping patients’ confidence.”
When providers embrace ‘privacy by design’ principles—meaning the integration of privacy at every stage of development for new features—they can comfortably scale their digital offerings without breaching confidentiality or damaging patient confidence, adds Shawky.
Providers must ensure these standards are also upheld by all ecosystem partners, whether insurers, health-tech companies, or device manufacturers.
Ali says, “This coordinated approach ensures that innovation doesn’t come at the cost of patient trust, enabling digital health solutions to scale safely while keeping patient privacy at the center.”
THE FUTURE OF PATIENT-CENTRIC TECH
Experts say that, over the next five years, technology will increasingly prioritize personalization, speed, and continuity of care. According to Shawky, AI-driven clinical assistants will shorten diagnosis times, remote monitoring will transform the management of chronic diseases, and telehealth will broaden access, particularly for underserved communities. Interoperable digital records will also help reduce fragmentation, creating “a much more connected and proactive healthcare system attuned to the everyday reality of the patient.”
Localized and targeted therapeutic delivery will be especially transformative in cancer care. By delivering drugs directly to the tumor site and reducing systemic toxicity, these approaches can enhance quality of life, shorten recovery time, and make treatment less disruptive, says Ali.
“This shift toward precision, minimally invasive therapy represents one of the most meaningful advances in patient-centric care.” He adds that remote monitoring, predictive analytics, and AI-enhanced clinical decision support will further strengthen these next-generation treatments.
The most profound changes will come from technologies that “feel almost invisible—working intelligently in the background to make care effortless, precise, and deeply personal,” says Sood, adding that AI scribes and agentic AI are already reducing administrative workload. “On a full day of the clinic seeing 30–35 patients, I am already saving nearly two hours of typing time. Agentic AI will enable systems that can think, act, and coordinate on behalf of both the doctor and the patient.”
According to Sood, these advances will help democratize elite medicine: diagnostic precision once reserved for world leaders, preventive protocols used by athletes, and longevity strategies adopted by billionaires will become widely accessible.
“When every person can have this level of medical attention, we’ll see a fundamental shift from sick care to genuine healthcare. That’s where healthcare is heading—anticipatory, frictionless, and intelligent.”