- | 9:00 am
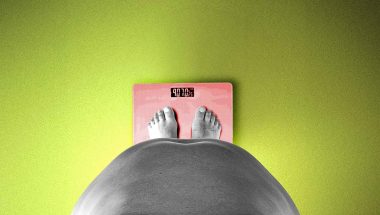
Obesity is a public health crisis in MENA—but how much is it costing the economy?
Experts say obesity, a growing regional health crisis, impacts health, and productivity.
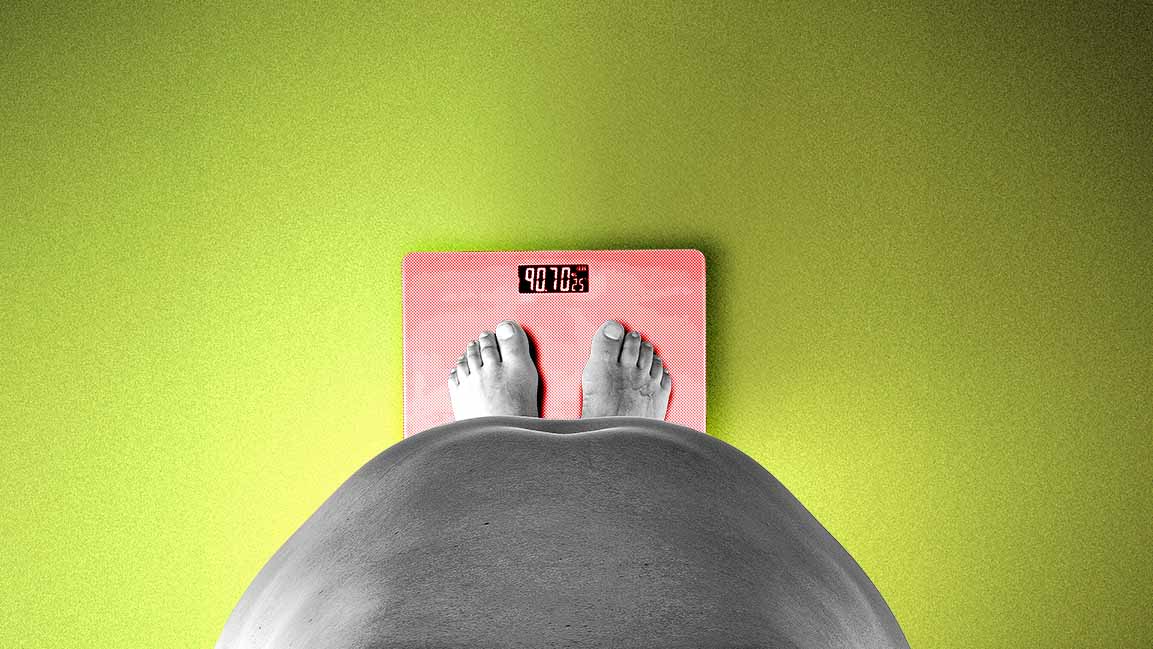
If you’re like many others, your goals for 2026 will likely include improving your fitness. And you should. Research indicates that waistlines in the Middle East and North Africa (MENA) region have been growing for decades.
Obesity affects 52 million children under 19 in MENA, according to a UNICEF report. Adult obesity rates in the region remain at 42 per cent.
An analysis in The Lancet found that weak responses to the obesity crisis over the years have caused a sharp rise in the number of people affected. By 2050, about one in three children and young people with obesity—130 million—are expected to live in just two regions: MENA and Latin America and the Caribbean.
This will have major health, economic, and social impacts.
STAKES ARE IMMENSE
It is a major crisis. But a race we can win.
“It affects societies, health, and productivity. In practice, this means obesity is becoming one of the region’s most pressing health challenges,” says Sumit Sharma, Head of Health and Life Sciences for India, the Middle East, and Africa at Oliver Wyman.
Obesity can lead to conditions such as diabetes, hypertension, and kidney disease—placing growing strain on health systems.
“It is associated with severe, life-limiting complications, reduced quality of life and premature death, with at least 2.8 million adults dying each year due to excess weight and obesity-related complications,” says Amr Saeed, Cardiometabolic Business Unit Head at Eli Lilly, META.
It also impacts mental health. People with obesity face higher risks of depression and anxiety, along with stigma, lower self-confidence, and barriers to social inclusion.
“The socio-economic impact of obesity is significant because it directly influences how fully people can participate in the workforce,“ adds Sharma. “As obesity-related conditions increase, many individuals struggle to sustain productivity, which inevitably affects economic output.”
Workplace bias and social discrimination can limit opportunities for people with obesity and may even discourage them from working. This leads to unnecessary exclusion and wasted talent.
“These dynamics impose broader societal costs — not only through higher healthcare spending, but through reduced economic contribution and diminished human potential,” Sharma adds.
In the UAE, about one in three adults has obesity. Rising obesity rates are costing the country nearly $12 billion each year.
“In the UAE, recent estimates put its economic impact at nearly $12 billion annually, with costs projected to approach 5 percent of GDP by 2035,” says Khalid Ghaloua Adine, CRO at Rain Stella Technologies. “It erodes productivity, strains health budgets, and amplifies risks of diabetes and cardiovascular disease — patterns consistently reflected in regional health data.”
GOVERNMENT REGULATION AND CORPORATE ACTION
The UNICEF report warns that diets high in unhealthy, ultra-processed foods are causing high rates of overweight and obesity among children and teens in MENA. Junk food is replacing healthier options.
Experts say that to control the costs of the obesity epidemic, both government regulation and corporate action are needed. Steps like the UAE’s tax on sugary drinks and stricter food standards in schools are essential first moves.
In the UAE, there are also system-level efforts. MoHAP’s 2025 National Clinical Guideline for adult weight management reframes obesity as a chronic disease and standardizes care pathways nationwide.
“Its guideline has been adopted across major health systems, signaling a shift toward chronic disease management while demonstrating how robust data infrastructure and interoperability can translate awareness into measurable health outcomes,” says Adine.
In Saudi Arabia, where more than a quarter of adults are obese, especially women, the Ministry of Health and the Saudi Food and Drug Authority are making obesity prevention a priority under the National Health Transformation Program and Vision 2030. Their focus is on health promotion, better diets, and creating spaces that encourage physical activity.
CURBS ON JUNK-FOOD MARKETING?
However, across the Gulf, Adine says, “We still see heavy promotion of high-sugar, high-fat foods, while regulation remains uneven.”
To address rising childhood obesity, some experts advocate for food-marketing restrictions like those recently adopted in Britain. Since January, unhealthy foods and drinks have been banned from online ads and TV before 9 pm in the UK to shield children from junk food advertisements. Additionally, major supermarkets can no longer run volume deals, such as “buy one, get one free.”
“Stricter curbs on junk food marketing are essential, particularly to safeguard children and adolescents,” says Narjesene Rasheed, expert dietitian and nutritionist at Kaya Clinic, Dubai.
“Regulations should include limits on digital advertising, clearer nutritional facts displayed on restaurant menu cards, and guidance on portion size control. Such measures can counter misleading promotions, encourage informed choices, and support healthier eating behaviors across the population,” adds Rasheed.
Change is underway.
Abu Dhabi’s 2024–25 standards now restrict unhealthy food advertising in and around schools and public spaces, and Saudi Arabia’s Food and Drug Authority has issued guidance on marketing to children. “Extending such mandatory, nutrient-based rules region-wide — and using digital platforms like ours to monitor compliance — would be a powerful lever alongside taxes and labelling reforms,” adds Adine.
RISE OF WEIGHT-LOSS DRUGS
Until recently, options for treating obesity were limited to either surgery or lifestyle changes like eating less and exercising more. The introduction of GLP-1 weight-loss drugs, such as semaglutide, changed this. Reports say that affordable generic versions and new pill forms will make 2026 the year weight-loss drugs become widely available.
MENA will play a key role in this change since the region has about 80 million adults with obesity. This makes it a major potential market.
Saeed says Lilly—having committed more than $55 billion since 2020 to build, expand, and acquire manufacturing facilities—continues to “see extraordinary demand for its innovative incretin medicines and is shipping more than ever to meet it.”
The rapid growth in the weight-loss drug market is driven by high obesity rates, greater awareness, and demand for fast results.
“New pharmacological treatments have gained popularity, particularly in urban populations,” says Rasheed. “While beneficial for selected patients, this growth underscores the need to prioritize prevention, portion control, nutrition education, and sustainable lifestyle interventions alongside medical therapies.”
In the MEA region, the obesity drug market was worth $149.06 million in 2024 and is expected to reach $671.67 million by 2030.
“Growth rates far outpacing traditional pharma categories, especially for GLP-1-based therapies,” says Adine. “In the UAE alone, GLP-1 revenues are expected to more than double between 2024 and 2030, growing at roughly 14% a year from a 2024 base of about $137 million — a trend already impacting payer budgets and provider prescribing patterns.”
However, a new BMJ study led by University of Oxford researchers shows that people who stop taking weight-loss injections regain all the lost weight within two years — faster than those on other weight-loss approaches.
The findings underscore that while these drugs are a powerful new tool, they are not a magic fix. “Medical treatment must be integrated into individualized, physician-led care plans and supported by structured lifestyle measures,” says Saeed.
Long-term success requires comprehensive behavioral and lifestyle support, including healthier diets, regular physical activity, and systemic changes to the food environment — from reducing junk-food marketing to improving the affordability and availability of healthier options.
“We’re now at an inflection point, the trends are clear, but early, coordinated action can still shift the trajectory before it becomes a much larger crisis,” says Sharma.
This means promoting wellness, supporting healthier lifestyles, and ensuring those with obesity-related conditions have access to effective clinical care, from structured diet and lifestyle programs to medical treatment.
Stressing stronger obesity management policies, Saeed says national frameworks should recognize obesity as a chronic disease, be grounded in clear evidence, and ensure equitable access to care.
“Collaboration across policymakers, healthcare providers, employers, and the wider ecosystem is critical to building durable, scalable, and economically aligned solutions,” Saeed says, adding that as scientific understanding advances, obesity must be managed with the same rigor and clinical discipline as other chronic diseases.
Emphasizing that taking obesity seriously today is an investment in a more productive workforce and the region’s long-term economic resilience, Sharma urges, “We must act immediately to give the region the best chance to support healthier, more engaged populations and avoid far more serious consequences down the line.”