- | 9:00 am
Bringing a missing sense of touch to surgeries. Middle East researchers develop a tool
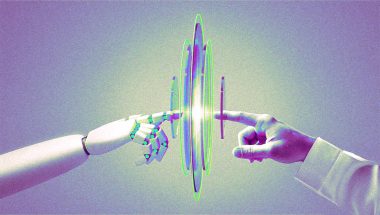
Researchers at the New York University in Abu Dhabi have created smart forceps that allow surgeons to feel internal tissues remotely.

Wonder how doctors now perform surgeries without needling into your skin? When Dr Asrar Malik uses a laparoscopic grasper to reach internal organs through a small incision for non-invasive surgeries, he only has an endoscope to see what’s happening inside. While such procedures prevent scars caused by open surgeries and mean a less painful recovery for patients, they make the surgeon’s job harder. Having a 3D view of the part being operated on sounds convenient, but the fact remains that visuals don’t make up for the absence of the sense of touch.
This means that with a tiny camera inside the body, surgeons make decisions during surgery partly based on intuition, sensing the movement or stiffness of tissue. Needles, graspers, and tubes can’t convey the sensation that direct touch can, which has remained a challenge for keyhole surgeries. As the world moves towards telemedicine, it will be crucial to make up for this absence of touch.
“For minimally invasive surgery, surgeons have no resources other than indirect contact with the surgical site and organs using long surgical tools that limit touch sensation. Therefore, they tend to depend on visuals to judge tissues and decide actions throughout the surgical procedure. This skill is difficult to develop even after many years of experience,” says Mohammad Qasaimeh, associate professor of Mechanical Engineering and Bioengineering at New York University, Abu Dhabi.
Thermal imaging based on infrared has provided surgeons with an enhanced view of internal organs for minimally invasive surgeries (MIS). Virtual reality headsets have entered the operation theatre and are now facilitating remote collaborations between surgeons from different parts of the world.
Similarly, there are metaverse surgeries, where doctors can rehearse procedures on a 3D model of the patient’s body, to be better prepared to make quick decisions. The same can transform the learning process for medical students, who can enter operation theatres remotely in real-time without interrupting the surgery.
But, while all these solutions allow surgeons to visualize the procedure, they still lack the sensory insight essential for split-second decisions during an operation. So how does one ensure that the sense of touch matches the progress achieved in integrating visual data and AI into healthcare?
EVOLUTION OF THE IDEA
Imagine if a surgeon could feel the tissue and internal organs without touching them directly. Beyond surgeries, what possibilities can that open up for remote consultations and procedures when a patient needs to be in isolation?
Researchers at the New York University, Abu Dhabi, have explored the possibilities by developing a tool that fills in for the absence of the touch sensation in keyhole surgeries. They have embedded sensors onto laparoscopic graspers that depict the tissues’ stiffness and how internal organs feel to doctors holding the device. This prototype for smart laparoscopic forceps solves a major dilemma for surgeons caused by a limited field of vision despite the use of cutting-edge imaging.
Tactile information relayed through the sensors on graspers provides real-time insights for surgeons to make quick and informed decisions.
“Surgical actions, such as handling, manipulating, stitching, or cutting tissues, would ultimately manifest improved efficiency to achieve better outcomes if aided by our proposed smart feedback system,” says Qasaimeh.
“Based on Hooke’s law of elasticity, estimating the tissues’ stiffness and detecting the presence of hidden lumps were validated in our study while reducing the magnitude of applied forces and required time. All these adding-up factors can enhance the surgeon’s precision during MIS,” he adds.
But while this has been developed for minimally invasive surgeries and is still just a prototype, it’s natural to wonder if there’s potential to enhance telemedicine or remote surgeries. The Middle East has already witnessed robotic arms for surgeries that can be controlled from a distance. Qasaimeh elaborates how “Robotic surgery systems can be used in telemedicine, where the surgeon does not have to be on the surgical site. However, these systems also suffer from the absence of real-time tactile force feedback, and hence the same ‘lost sense of touch’ dilemma remains.”
He hopes that “developed technology can be introduced to robotic surgeries, where information on force and stiffness can be sent back to the surgeon for higher precision and shorter operations.”
Different samples underwent tests with multiple surgeons to check this innovative surgical tool’s efficiency. Going into detail, Qasaimeh says, “Surgeons were asked to manipulate and sort chicken and sheep samples based on their stiffness. Expert surgeons sorted the samples more efficiently and in a shorter time when they used the developed smart forceps compared to using the tool with only visual judgment. On the other hand, less experienced surgeons found the developed tool necessary for sorting the samples successfully.”
EXPLORING NEW HORIZONS
Trends such as streaming surgeries live and collaborating in virtual reality are becoming the future of healthcare. The online medical data allows patients to consult doctors in other countries and practitioners in different locations to share information for providing better care.
Dr Shafi Ahmed, director of Medical Realities, who became the first to stream a surgery using Google glass in 2014, says, “A lot of the technology now can work on low bandwidth and stream, so you can do telementoring or train (surgeons) remotely.”
While the above solutions thriving on higher connectivity can provide visual support for surgeons and medical students, can Abu Dhabi’s New York University’s sensors introduce a sense of touch?
Qasaimeh is positive. “The tactile feedback displays the measured grasping forces and deformation angles in real-time, which get translated into meaningful estimates of the tissue’s stiffness characteristics, and consequently, used for tissue/organ health classifications.”
As for medical students, these smart forceps can be the next step toward increasing their precision during surgery remotely.
“Integrating tactile feedback systems with devices in the simulation center would help trainees reduce their learning curve and provide smart tools to prepare them for actual surgeries effectively,” adds Qasaimeh.
Even as the possibilities are many, there is still time for the device to make it to market. Although it has been proven effective, Qasaimeh says, “This serves as a pre-step to test new concepts before developing novel sensors with strict requirements that satisfy the FDA regulations.”
“Once thriving, products incorporating artificial tactile sensation are expected to attract high interest, and the demand will increase, especially for robot-assisted and teleoperated surgeries,” he adds.