- | 9:00 am
There’s new hope for millions in MENA suffering from diabetes-related conditions
Abu Dhabi Stem Cells Center is developing innovative treatments using human-reprogrammed skin and blood cells
On his good nights, Ahmed Ahmed, a Dubai-based retiree, dreams of dune bashing again. On bad ones, simply lying on the bed triggers sleepless agony. He suffers from acute diabetic pancreatic beta cell dysfunction, whose complications include chronic kidney disease, cerebral infarction, and myocardial infarction. This afflicts 537 million individuals worldwide who have diabetes. Unable to even walk around the block, Ahmed is finding managing his diabetes a very complicated process. Even the best situations are hard to manage for people with diabetes.
The prevalence of diabetes in the UAE was reported by the International Diabetes Federation (IDF) to be 16.3%. Research shows that diabetes has the highest regional prevalence in the Middle East and North Africa.
Fortunately, a collaboration is poised to revolutionize diabetes care by developing a new innovative treatment using pancreatic beta cells derived from human induced pluripotent stem cells (iPS cells). iPS cells are obtained from skin or blood cells and then reprogrammed (genetically modified) in highly advanced laboratories to create cells replicating the tissue affected by diabetes.
PERSONALIZED SOLUTION
This joint research is led by Abu Dhabi Stem Cells Center (ADSCC) with Asia’s top research institutions, Kyoto University – Center for iPS Cell Research and Application (CiRA), and Rege Nephro, a Japan-based biotech company.
“Our joint research will pave the way for creating replacement beta cells that match the patient’s needs, potentially offering a long-lasting solution to insulin deficiency in type 1 diabetes and even exploring regenerative pathways,” says Prof. Dr. Yendry Ventura, CEO of ADSCC and Adjunct Professor at UAE University.
RESTORE INSULIN PRODUCTION
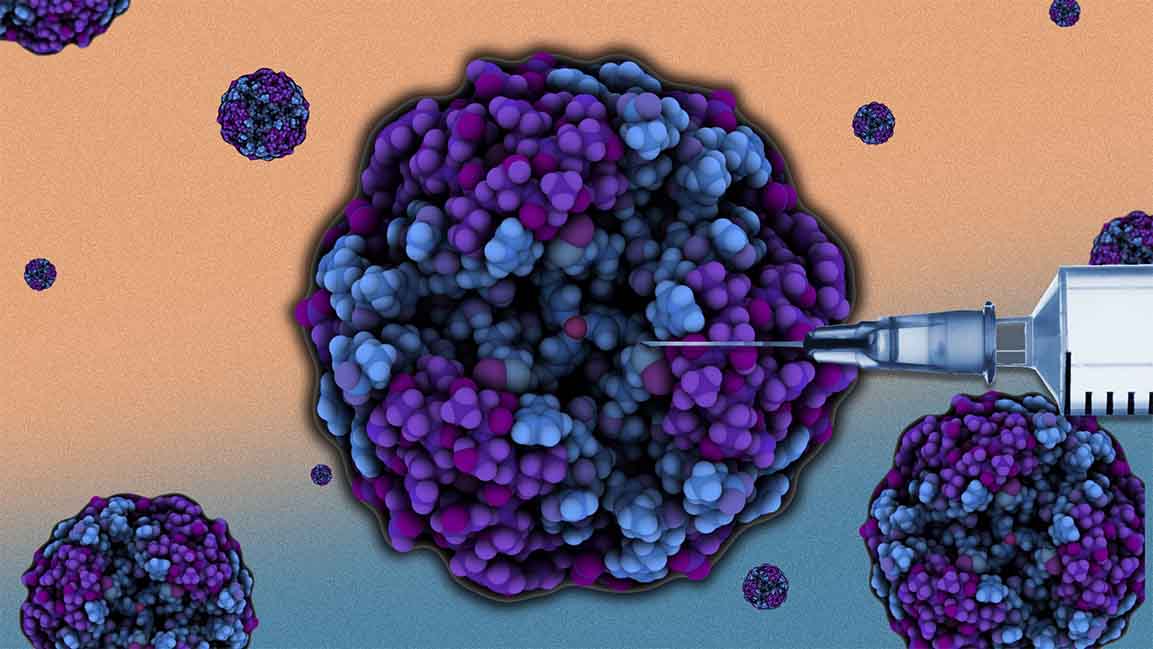
The research will focus on developing iPS cell-derived pancreatic beta cells with enhanced therapeutic efficacy through genetic modifications, offering cell therapy options for patients with type 1 diabetes, where the body’s immune system mistakenly identifies and damages the insulin-producing beta cells in the pancreas.
“The research aims to develop a new therapy to restore insulin production by developing replacement beta cells derived from patient-specific stem cells, mainly skin and blood cells, potentially reducing or even eliminating reliance on daily insulin injections in the future,” says Ventura.
The research will also explore novel approaches for type 2 diabetes, where beta cells might exhibit dysfunction rather than complete destruction. “Through drug screening and testing, we aim to identify new therapeutic targets and develop more effective management strategies for this complex form of the disease.”
ADSCC has established a dedicated laboratory within Kyoto University premises to facilitate this joint mission for knowledge exchange and technology transfer, which Ventura says will cement ADSCC’s role and mission in the Middle East and North Africa in leading regenerative medicine and cellular therapy research.
“Given the high prevalence of diabetes in our region, this collaboration allows us to support the specific needs of our population,” he says.
He adds the ultimate goal is to revolutionize diabetes care by offering personalized, curative solutions for both type 1 and type 2 diabetes.
“Imagine a future where patients with type 1 diabetes don’t have to rely on daily insulin injections, and where those with type 2 diabetes have access to more effective and personalized treatment options that prevent complications and improve their quality of life.”
MULTI-PRONGED APPROACH
In recent years, although a variety of technologies have hit the market for patients with diabetes, but still, the disease is overwhelming for many. This is partly due to the complex nature of diabetes, Ventura says, with different subtypes and causes. “While some technologies work well for certain patients, they might not be as effective for others. Accessibility and affordability also play a crucial role.”
Beyond technology, there are challenges related to patient adherence and lifestyle factors. Managing diabetes effectively requires a consistent commitment to medication, diet, and exercise, which can be challenging for various reasons for patients.
“As healthcare providers, we are responsible for continuing our research and trials to discover and develop new treatments and cure diseases such as diabetes,” says Ventura. “That’s why we believe a multi-pronged approach is key – developing innovative technologies using cellular therapy while addressing wider accessibility issues and supporting patients in their daily disease management.”
Besides this collaboration, ADSCC is also working on other projects related to diabetes, including its ongoing clinical trial to evaluate the efficacy of extracorporeal photopheresis (ECP) in the treatment of type 1 diabetes and develop a new vaccine that aims to teach the body’s immune system to be more tolerant towards pancreatic tissues.