- | 8:00 am
Full-body MRI scans are getting popular. A doctor weighs in on the pros and cons
A 25+ year veteran of medical imaging research says that while the debate rages, he’s much more interested in how we can reinvent these tools as part of a new kind of regular physical exam aimed at keeping people everywhere healthy.
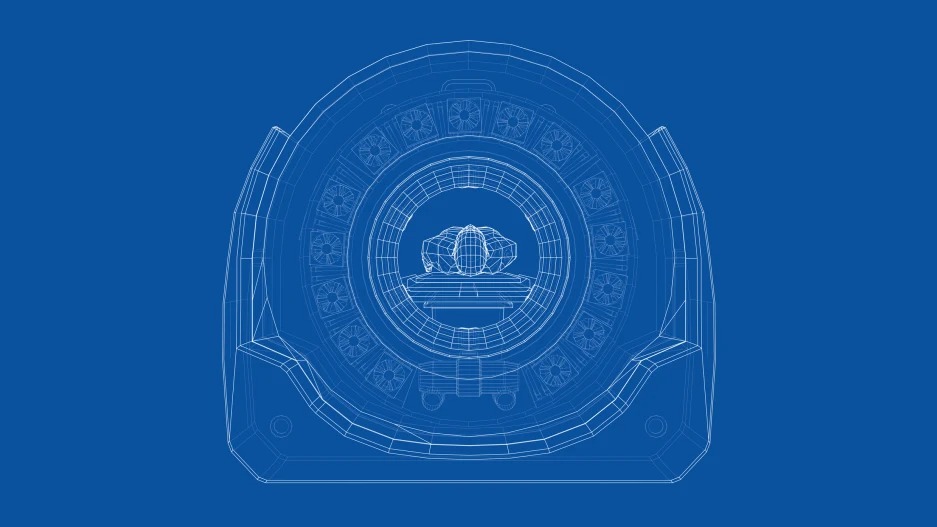
Most of us are familiar with magnetic resonance imaging, or MRI. The MRI is a noninvasive medical imaging test that produces detailed images of internal structures in the human body, including the brain, the heart, abdominal organs, muscles, blood vessels, ligaments, and bones. MRI scanners create these images using somewhat surprising tools: radio waves and a strong magnet.
Historically, MRI has principally been used for the diagnosis and characterization of disease once other signs and symptoms have developed. A referral from a physician is usually required to get a scan. In other words, we use MRI when we become aware, through other means, that a problem already exists.
A new crop of companies such as Prenuvo is beginning to offer consumers direct access to full-body MRI scans as a means of proactively monitoring for potential disease. Ezra, for which I am a scientific adviser, is among them. The rise in adoption of this new service among celebrities and influencers—people with disposable income and a predisposition to try anything new that promises to increase health and longevity—has sparked a public debate. Do the benefits of proactively screening the whole body outweigh the potential drawbacks?
More specifically, do these scans trigger too many false-positive results, leading to unnecessary and expensive follow-up tests, unwarranted surgical procedures, and needless anxiety in otherwise healthy people?
I have been a medical imager for more than a quarter of a century now. In that time, I have seen MRI machines and other scanners get sleeker, faster, and better. I have also seen the arguments over imaging-based screening play out time and time again, just as we are seeing now. I have come to believe that it is time for a different kind of dialogue.
The argument among screening enthusiasts is clear: Early detection saves lives. Recent data assembled by the American Cancer Society, for example, indicates that the five-year survival rate of cancer on average changes from 20% to 80% if it is caught early. This suggests that early detection for all would result in billions of lives saved around the globe. Trillions of dollars in downstream healthcare costs would be saved as well.
The classic retort among circumspect medical professionals (a retort I myself have uttered many times before) is that imaging, in particular, should be used for screening only in those with a significant known risk of disease—due to a prior diagnosis or a genetic predisposition, for example—because only in these cases will the benefits of early detection outweigh the risk of false positives. Studies have cast doubt upon the balance of risks and benefits even for established general-population screening tests such as mammograms.
The medical profession is right to be concerned about indiscriminate screening performed without consideration of risk-benefit tradeoffs. It is also important, though, not to assume that imaging can only be done as it has been done in the past. As I mentioned, imaging technology changes, as does clinical practice. An interesting example of such a shift has quietly been taking hold in medical circles in recent years. Among select populations, such as people with a moderately elevated risk of breast cancer, prostate cancer, or lung cancer, the medical community recommends something called “active surveillance.”
Active surveillance involves regular imaging of specific body parts to monitor for new signs of disease. A key component of active surveillance programs is repetition. If doctors are imaging you regularly, they can afford not to do a full-court press for every uncertain finding, since they know you will be back for another imaging session before long. More than that, the rate at which false-positive results are found can actually drop with regular imaging. The more often imaging professionals see you, the more they understand what is normal for your body, and the more data they have for comparison. Many concerns that might otherwise lead to follow-up tests and procedures can be ruled out immediately if suspicious findings appear unchanged compared to previous findings.
For active surveillance of breast cancer in people with selected risk profiles, MRI is now preferred over mammography, despite the fact that the false-positive rate for a one-off MRI scan is still higher than those of us who work on MRI might like. For breast MRI and prostate MRI both, radiologists now use numerical rating systems (called BI-RADS and PI-RADS) that are specifically designed to quantify cancer risk based on imaging findings, helping patients’ physicians decide between continued periodic imaging and more invasive follow-up procedures like biopsy or surgery.
What does the example of active surveillance tell us about the advisability of full-body imaging? It tells us that there is another way to think about imaging tests, not just as one-off diagnostic procedures, or “screens” that display a single snapshot, but as part of a disciplined program of longitudinal monitoring over time. The longitudinal aspect is essential. So is the discipline.
Ezra, for example, evaluates your risk for various types of cancer prior to scanning, uses standard-of-care MRI protocols designed for active surveillance in each individual organ or body area, employs trained radiologists who use established rating systems to track change after each scan is done, and deploys artificial intelligence (AI) to accelerate the process and clarify any findings. Previous clinical trials don’t really speak to the risk-benefit balance for full-body imaging when it is performed in this way.
When it comes to the question of whether full-body MRI is a good or bad idea, then, here’s the rub. It continues to be a bad idea if it is done wrong, but it can be a transformatively good idea when it is done right.
Isn’t it time, then, that we started doing it right? First and foremost, we need to document carefully the results we get when we monitor otherwise healthy individuals with care over time. The best way to rule out false positives is to image more frequently, but until now, we as a society have not been imaging frequently because we are afraid of false positives (and associated costs). We can debate until we’re blue in the face, but, if we want to make a real difference in preventive health, we need to break this cycle.
Active surveillance programs have already given us a base of experience to work with, and new technologies like AI are already starting to help, allowing us to connect scan sessions ever better over time, and even enabling us to develop cheaper scans and design more accessible scanners. The landscape of costs is changing, as is the breadth of potential benefits. The future of imaging does not look the same as its past.
The debate between physicians and tech influencers may continue to rage, but I am not as interested as I once was in the nitty-gritty details of the debate.
For all the years I have worked with MRI machines, I have been frustrated that these devices, which are some of our best tools for identifying disease, are used only for people who are already sick.
Now, I am much more interested in how we can reinvent these tools as part of a new kind of regular physical exam aimed at keeping people everywhere healthy.