- | 8:00 am
How this company’s AI tools help prevent suicide and mental health crises
NeuroFlow’s platform uses natural language processing to evaluate suicide risk in patients.
Suicide rates are on the rise. Nearly 50,000 people died by suicide in 2022, a 3% increase from the previous year according to the CDC, and a 36% increase since 2000. Not only is suicide traumatic; it’s expensive. During 2015-2020, suicides and self-harm cost an average of $510 billion a year.
Yet, the health system is ill-equipped for suicide prevention. Clinicians and healthcare providers are hamstrung by a lack of technology for managing suicide risk. Typically, if someone needs help for a mental or emotional disorder, they are given an assessment at a clinician’s office to gauge their risk for suicide. One of these is the Patient Health Questionnaire-9 (PHQ-9), which measures the severity of someone’s depression and ends by asking them how often they have thoughts about self-harm or suicide. If the patient doesn’t come back, providers don’t have a window into understanding how the patient is doing, or determining who is at high risk and needs follow-up care. It’s easy for patients to fall through the cracks.
Christopher Molaro wants to use AI to change this. In 2017, he founded NeuroFlow, a technology platform that behavioral healthcare providers can use to keep track of their patients and assess their suicide risk. Molaro, who served in Iraq, decided to focus on suicide prevention after one of his fellow soldiers died of suicide.
“It felt like a leadership failure—we made it through 12 months of combat, then someone dies at home,” he said.

Patients, who are enrolled in NeuroFlow via their health insurer, have access to an app, where they receive the PHQ-9 and other assessments such as the GAD-7 for anxiety, which their clinician deems necessary at regular intervals, and can also journal. To incentivize engagement, the app rewards users with points that can be redeemed for gift cards (depending on the provider) whenever they log mood or sleep, answer questionnaires, add journal entries, and complete modules.
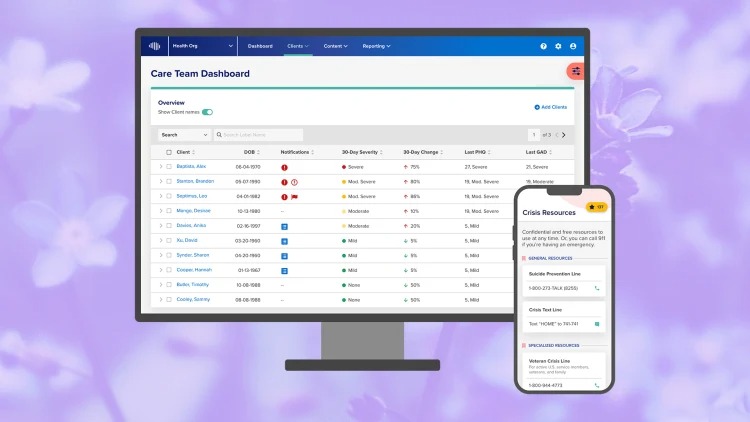
NeuroFlow is able to use natural language processing to analyze the journal entries for increases in a patient’s suicide risk. On the back end, healthcare providers see a dashboard listing all of their patients. NeuroFlow analyzes patient data from assessments and journal entries and can alert providers about patients in urgent need or changes to a patient’s mental status.
Since 2021, insurer Prudential has been using NeuroFlow’s capabilities to power a suicide-prevention program that allowed patients receiving disability benefits to track their sleep, mood, and levels of pain. Case managers at Prudential received alerts when someone was at risk of a mental health crisis and were then able to contact the patient about next steps that include therapy or the local hospital.
Since the program started, NeuroFlow has alerted Prudential to 1,200 people at risk for suicide, and enabled interventions that helped bring a 34% decline in depression after triggering an alert. “The disability population is particularly vulnerable to mental health challenges,” Dr. Kristin Tugman, vice president of holistic wellness at Prudential, told Fast Company via email. “We’ve able to meet them where they are in their needs and provide meaningful resources to them at a difficult time.”
Beyond suicide prevention, NeuroFlow’s clients are helping investigate other ways the platform can be used to improve mental health care delivery. Behavioral health provider Magellan Healthcare was an early investor in NeuroFlow, contributing $20 million to its series B round in 2021. That’s when Magellan started using the tool as it moved toward a collaborative care model allowing a patient’s care team—psychiatrist, primary care provider, and case manager—to share information and communicate with each other about the patient.
“We couldn’t scale it quickly before NeuroFlow because we didn’t have the technology,” said Dr. Caroline Carney, chief medical officer at Magellan. She pointed out that psychiatrists are often overbooked and it can be difficult to get an appointment with them. In a collaborative care model, the psychiatrist can recommend treatment plans to a primary care physician who can then write the prescription for the patient.
“With NeuroFlow we’re able to screen and catch issues more efficiently and get patients into care earlier,” Dr. Carney says. Last year, Magellan collaborated with NeuroFlow to create a platform with cognitive behavior therapy programs aimed at improving mood, mindfulness, and sleep. It found that registration was 124% higher than previous programs, there was a 41% reduction in anxiety assessment scores, and a 24% reduction in depression scores based on PHQ-9 results. In March, Magellan created a similar program for teens between the ages of 13 and 17.
According to Molaro, in 2023, NeuroFlow alerted its clients to 33,000 people who were at risk of suicide, who he says may have otherwise slipped through the cracks in the healthcare system. Currently, NeuroFlow is available in all 50 states and has 15 million lives under contract.
“A lot of this is not new,” Molaro said. “It’s about how to make validated clinical assessments more engaging and scalable. The triple bottom line is to get people better, reduce cost, and make it sustainable by freeing up resources.”