- | 9:00 am
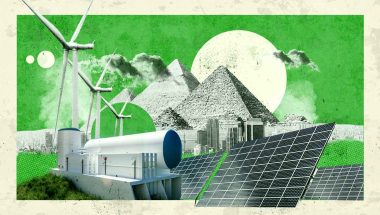
Allergy season in the Middle East is getting worse. Blame climate change
Mounting evidence shows the link between climate change and prolonged pollen seasons. What does this mean for those more prone to allergies?

For some of us, walking in the grass may be a relief from the scorching summer. For others, summer may mean sneezing and coughing, popping antihistamines, a box of tissues, and a trip to the doctor. Unfortunately, due to climate change, allergies are only getting worse.
“Since mornings were characterized by intense coughing and sneezing, my ENT specialist advised me to use Seretide every two days. I don’t have asthma, but due to severe dust allergies, my inhaler has become commonstay,” says Audrey Reynolds, a resident in the UAE.
Reynolds’ experience is emblematic of many in the region.
“The Middle East is facing one of the hottest summers this year, with temperatures soaring to 51°C. What this implies is increased humidity triggering more pollen release from grass and trees, added to the dust in the air, which gets aggravated by the frequent sandstorms,” says Dr. Raviraj, Specialist Internal Medicine, Aster Clinic, Muteena (DMPC).
A growing body of research provides substantial evidence of climate change’s contribution to rising allergies. According to the findings outlined in the Extreme Allergies and Climate Change report, the increasing temperatures are expected to extend the duration of allergy seasons while simultaneously deteriorating air quality. As per the report, prolonged allergy seasons have the potential to result in a higher prevalence of allergies and a heightened risk of asthma attacks.
This connection between climate change and allergic conditions underscores the importance of addressing environmental factors in healthcare planning and policy decisions.
NOT JUST A COMMON COLD
The influence of climate change on respiratory health is well known. However, our understanding of the long-term trends in continental pollen distribution and of climate change in shaping these patterns warrants further investigation.
Research efforts by William Anderegg of the University of Utah School of Biological Sciences studied the linkage between climate change and pollen season in the US. “The strong link between warmer weather and pollen seasons provides a crystal-clear example of how climate change is already affecting peoples’ health,” Anderegg says.
Meanwhile, Dr. Raviraj says that while research is limited, a growing number of respiratory issues are attributable to increased pollen and dust particles, which, in turn, can exacerbate in individuals with reactive airways.
“Consequently, we observe increased asthma and chronic bronchitis during this season,” he says.
Reported respiratory allergy cases are characterized by a dry, irritant cough and symptoms such as a nocturnal cough disrupting sleep, wheezing, shortness of breath, and chest congestion.
Dr. Raviraj explains that hay fever, or allergic rhinitis, is prevalent in the current climate crisis. This condition typically presents with symptoms such as nasal stuffiness, a runny nose, sneezing, red and itchy eyes, and excessive watering.
Moreover, pollen can affect the skin in several ways. Dr. Raviraj points out that the combination of heat, humidity, dust, and pollen can also trigger eczema in individuals with sensitive skin conditions like lichen planus or psoriasis. These reactions manifest as intense itching and actively oozing skin lesions.
COULD IT BE WHERE YOU LIVE?
Heat, humidity, and pollen aren’t the sole culprits behind allergies; there’s more.
In densely populated cities, where daily traffic congestion is a common sight, the prevalence of allergies is significantly heightened.
The pollution generated by heavy traffic plays a significant role in exacerbating allergies, says Dr. Raviraj. He emphasizes that ground-level ozone, a hazardous pollutant, is formed from precursors such as nitrogen oxides (found in automobile exhaust) and volatile organic compounds (VOCs) in the presence of sunlight. This has been directly linked to asthma and atopic dermatitis.
A study by the National Library of Medicine examined the connection between exposure to air pollutants from traffic and respiratory ailments in children. Among the numerous discoveries it unveiled, one finding indicated that school children residing near major roads (within 50 meters of trunk roads) exhibited a higher prevalence of asthma when compared to their counterparts living in rural areas. Such research in Middle East countries is limited.
Dr. Raviraj explains that exposure to ozone, as demonstrated in human experiments and animal models, leads to impaired pulmonary function, heightened airway responsiveness, and increased lower airway inflammation.
Additionally, ozone indirectly interferes with mucociliary clearance and triggers the production of free radicals.
In the context of traffic-related air pollutants, Dr. Raviraj highlights that particulate matter, whether in solid or gaseous forms, are triggers of asthma and allergic rhinitis attacks. These pollutants are notorious for causing airway irritation and inflammation, contributing to allergy-related health issues.
The relationship between climate change and allergies presents a compelling narrative of environmental shifts impacting human health. As we witness rising temperatures, increased humidity, changing pollen patterns, and the proliferation of air pollutants, allergies have become more pervasive.
While the implications of climate change on allergies are complex and multifaceted, there is a pressing need for awareness, adaptation, and mitigation strategies. As Anderegg asks, “Climate change is in every breath we take. The biggest question is—are we up to tackling it?”