- | 8:00 am
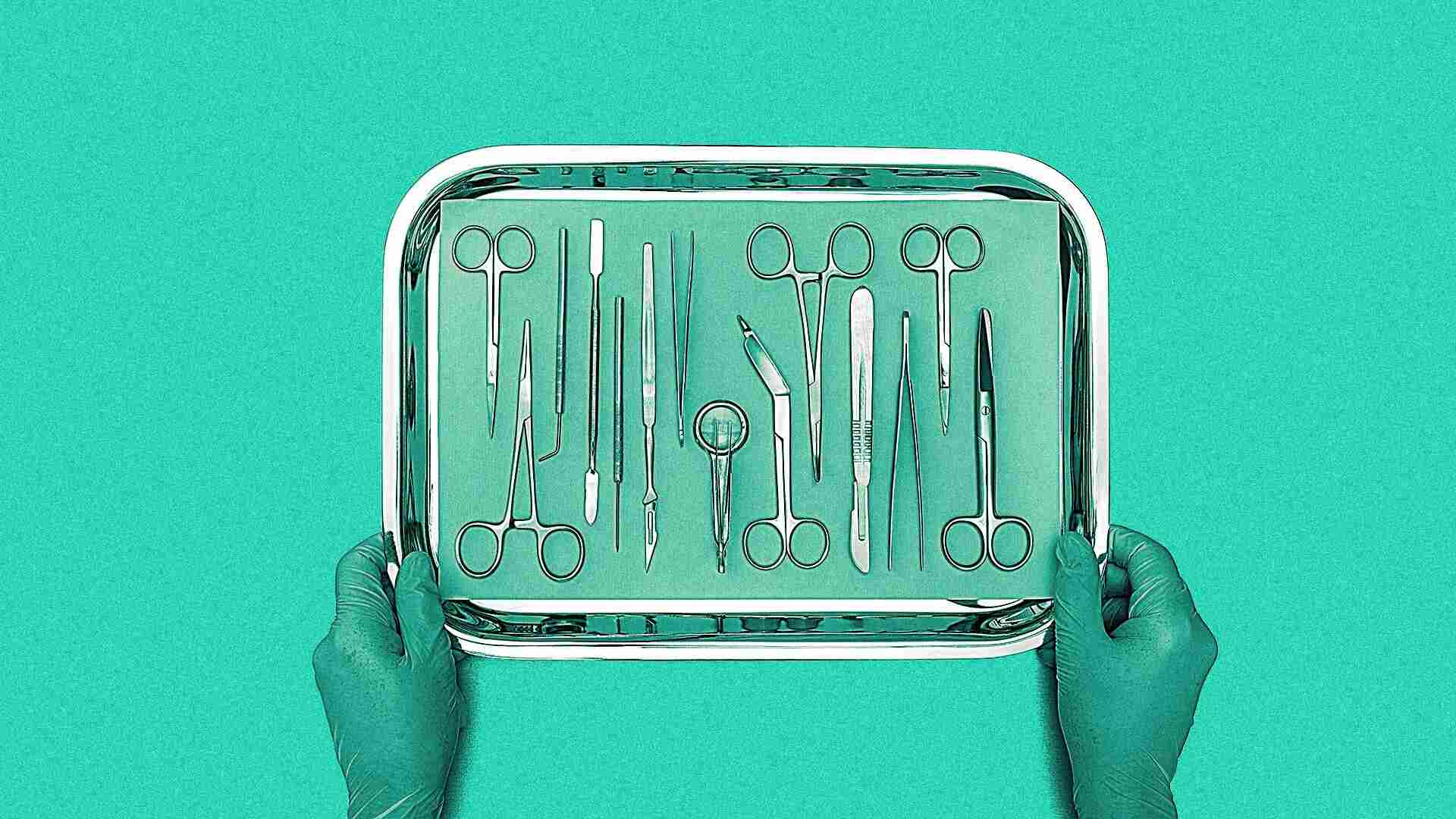
Surgery outcomes can vary wildly for the same procedure. This AI platform is changing that
By analyzing video footage of surgeries, Theator can help identify steps surgeons can take to improve post-op outcomes.
When Dr. Tamir Wolf diagnosed his wife and a former boss with appendicitis in 2016, he referred each to a different hospital for their appendectomies. Though his wife was in and out within 12 hours and had a smooth recovery, his boss nearly died.
“It was mind-boggling,” Wolf says. “They had very similar situations, very different decisions, very different treatments and very different outcomes.” In an effort to reduce outcome disparities between hospitals and even surgeons, Wolf launched Theator in 2018 to use AI as a method to help improve surgeons’ skills.
Despite how complex surgery is, the typical operating room is a black box. No one knows what happens in a surgery except for the surgical staff, and there isn’t anyone providing feedback in the moment or afterwards.
The way that surgeons are trained means that they tend to emulate whoever taught them—for better or worse.
“You become the kind of surgeon that your mentors trained you to be,” says Dr. Danielle Walsh, professor of surgery and vice chair of quality and process improvement at University of Kentucky. “Their biases, suture choices, and how they think through an operation—that shapes you. You take those behaviors into your career where you practice independently.” In other words, most surgeons learn from very few people. Once practicing, they have few opportunities to get feedback on how to improve.
Theator attaches cameras to surgical scopes to film procedures. Its platform then analyzes the surgery alongside patient outcomes to determine what surgeons can do to reduce complications. It’s an approach that has raised the company $42.5 million in funding across three rounds—and laid bare shortcomings in surgery departments.
Last fall, the company highlighted research showing how certain practices in sleeve gastrectomies impacted patient recovery at four hospitals. More recently, at the American Surgical Asosciation’s annual meeting in April, research from Tel Aviv University showed Theator’s impact on gallbladder removal outcomes.
At the event, Dr. Gerald Fried, Chair of Board of Regents of the American College of Surgeons and a consultant for Theator, presented new research findings from the company and its results at Tel Aviv University. The research evaluated Theator’s impact on improving the use of best practices during surgery—which the platform found in use less often than surgeons expected.

“They thought they were doing this routinely,” Fried explained, describing the study. “When they did the study they realized they were only doing it about 40% of the time.” Once the surgeons started using Theator, adoption of such surgical practices as adopting a safety measure which minimizes injury to bile ducts jumped to 75%.
Beyond health impacts, Theator’s ability to identify surgical efficiencies also helps hospitals save money. University of Kentucky’s Walsh estimates that an operating room costs $60 to $100 a minute, depending on the type of the operation.
However, there are still barriers to adoption. One major one is the fear that tools like Theator will be used to penalize surgeons instead of help them improve. Dr. Walsh pointed out her institution was not able to use Theator because the legal risk team determined it was not adequately protected under Kentucky state law.
“[Surgeons] all make small errors, akin to hitting a curb when you are driving or having to repark your car to get it in between the lines,” she says. “The law needs to take into account what’s human error versus what’s truly a malpractice error that needs to be mitigated.”
Today, Theator is used in over a dozen hospital systems in the US, Canada, and Israel. Both Fried and Walsh compare Theator to the flight recorders that pilots use in the cockpit to record their conversations and settings for passenger safety.
“The aviation industry uses technology to monitor pilot performance for the safety of the public,” Fried said. “One day we’ll reach a point where it’s illegal to conduct a surgery without having it be filmed and analyzed. If we don’t adopt it first, it’ll be imposed on us.”